When is Therapy Inappropriate After Trauma?
- Odelya Gertel Kraybill

- May 14, 2018
- 6 min read

Therapists are often contacted by people who have recently experienced a “critical incident”. Accidents, crime, violence, death, illness, injury, and natural disaster are part of life everywhere. If caregivers are well-informed about the do’s and don’ts of responding to trauma, they can help reduce the consequences of such incidents for survivors, and perhaps mitigate the likelihood of developing PTSD.
Often those who approach a therapist for help after critical incidents - and even many therapists - are unaware that therapy should not be the first line of response after such incidents.
Meeting basic survival needs is, of course, the highest priority in crisis response. But as soon as the basics of safety, shelter, clothing, medications, food, and water, etc., have been addressed, there are additional needs requiring immediate attention that must precede therapy. These should be met by Psychological First Aid.
Psychological First Aid Immediately After Trauma
Psychological First Aid (PFA) is a short term set of support strategies that can be provided by anyone, clinician or not, who has gone through training for it, to support survivors to meet these additional needs. PFA has have been found to be effective in mitigating stress responses and assisting survivors to develop skills in coping with the after effects of trauma.
PFA provides immediate emotional support and care, gives information essential to understanding the psychological dynamics of stress and trauma, and connects people to needed resources. Various PFA frameworks exist. I’ve drawn on elements of several of them and field tested in several countries the following framework, for my Expressive Trauma Integration training:
Engagement. First communication was initiated, focus is on respect and compassion, especially in first interaction.
Establishing a sense of safety. Even when survivors are safe and basics of shelter, food, clothing, and medications are provided, due to the nature of stress responses to trauma they often don’t feel safe. Special effort must be made to address this. Providers approach this in differing ways. As an expressive therapist I am partial towards experiential methods and use of imaginal space* and experiential modalities to facilitate grounding and self-regulation.
Psychoeducation. Providing survivors with accurate information about how stress and trauma affect people is an essential step in normalizing their symptoms and managing what they are experiencing. Survivors also benefit greatly from a review of coping mechanisms found to be useful for addressing emotional, physical, mental, spiritual and social aspects of crises.
Identify vulnerabilities. Monitor immediate and anticipated vulnerabilities and risks. Survivors benefit from assistance in identifying their immediate vulnerabilities and how to address them. Care providers also need this info to assist in planning responses.
Reconnect to resources. Survivors often are not aware of their resources in times of crisis and need support in connecting to them, whether internal, personal, family, friends, communities, or services. It’s important to do this in ways that foster self-efficacy and a sense of control, connection and power, despite the limitations of the crisis situation.
Sustainability. The aftermath of a critical incident can last for a long time, during which stability and predictability are rare, and complex challenges are frequent. It’s essential to help survivors come up with short-term strategies and routines for emotional sustenance. Typically designed in a weekly framework, these provide emotional containment when there is no trained assistance available. They also help survivors move to the second stage of response – psychosocial support.
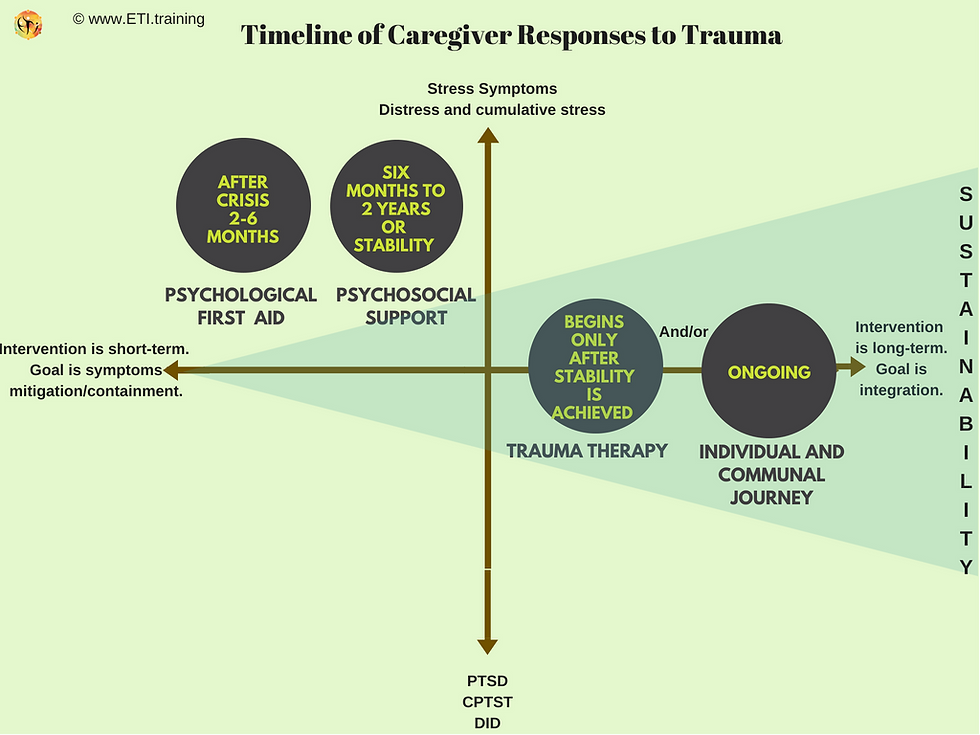
Psychological first aid is the first line of response from the time a crisis takes place until 2-6 months thereafter, depending on the situation. The next stage after PFA is psychosocial support, usually in a timeframe of up to two years after the crisis.
What is Psychosocial Support?
Whereas the above PFA responses have a goal of helping survivors cope for a short time, psychosocial support is designed to help meet medium to longer-term psychological and social needs of individuals and communities that commonly arise as they face adversities after crisis. A main goal of psychosocial support is establishing and maintaining a sense of stability in situations of instability.
In 2002, Psychologists for Social Responsibility published a report that provided guidelines for providing psychosocial support. The report recommended:
(1) a Do No Harm intervention approach, which highlights the importance of transitioning from a focus on pathology (highlighting the damage done by crisis) to a focus on wellbeing (resources and strengths of survivors). To accomplish this requires caregivers to consider all aspects of wellbeing as they conduct psychosocial support.
(2) Culturally sensitive intervention that considers the gender, religion, social structures, and beliefs about healing of survivors, and
(3) Sustainable Development, which requires that interventions address all aspects of wellbeing and thus must be linked to other basic services.
Expressive Psychosocial Support
In many previous blog posts I’ve emphasized the importance of using experiential modalities when addressing trauma. Trauma alters brain patterns, creating autonomic nonverbal responses that dominate conscious verbal thinking. A result is that survivors are often unable to translate their feelings and sensations into a narrative compelling enough to mitigate the stress symptoms and provide a sense of trauma integration.
This points towards interventions rich in use of bottom-up modalities that facilitate self-regulation and that individuals and groups can use on their own, when do not have access to therapists. Expressive Trauma Integration is an approach to therapy that employs many such modalities. These can be easily adapted to work with trauma survivors in what I call
Expressive Psychosocial Support.
Expressive Psychosocial Support should complement and continue PFA to the next level of intervention with a core objective of establishing and maintaining an ongoing sense of containment in circumstances of instability. Since in this stage stability has by definition not been achieved, therapy is not yet appropriate.
Why Psychosocial Intervention and Not Trauma Therapy?
A stable environment is a key requirement for trauma therapy to be effective. This means that psychosocial support intervention is often more suitable than therapy, even if trained trauma therapists are available.
Often survivors are living in situations where stability is not possible. Examples of such circumstances include: Children and teens in foster care, reunification processes, immigration before final settlement, refugee status, wartime, ongoing abuse, ongoing domestic-violence, short-term hospitalization (up to several months), etc. Right after trauma, survivors are consuming most of their resources just to cope with fear, change, and instability.
Survivors face not only the trauma and injury that may have come with it, but also don’t know when and how their crisis will end and what will follow. This means that survivors in such situations are still battling ongoing instability or unknown circumstances that require so much of their day-to-day internal and external resources that there is no capacity to conduct trauma therapy.
Therefore, it is important not to open the trauma story and the grief that accompanies it. The focus should rather be on support, compassion and encouraging self-compassion, with special attention to emotional containment and self-regulation activities.
Only after some clarity and stability have emerged regarding key life structures or decisions related to the trauma are clients ready to engage in trauma therapy.
What is Containment in Crisis Response?
In psychodynamic work, containment and holding refers to a mother enabling her child to express feelings and feel safe while doing so. In ordinary therapy the therapist acts as a container to hold the client’s feelings and thoughts, and processes them with the client to make them more understandable and less destructive (Finlay, 2015).
In early response to crisis, the concept of containment provides a useful reference point for caregivers. The focus of psychological first aid and psychosocial support interventions that follow should be to create and maintain a similar sense of holding and containing the emotional experiences of survivors over an extended period.
Especially in situations that lack stability and predictability, the goal should be to facilitate a sense of co-holding by the caregiver and client (in certain group settings, it might be between the client and a small group) and gradually to expand this to self-holding. Experiential modalities are particularly useful in promoting self-regulation and re-establishing a sense of containment in the midst of chaos.
In the image below you can see a timeline for trauma intervention.
Endnote:
*Imaginal space is an abstract creative space of play, fantasy, and spontaneity in which a client can explore and engage with different aspects of personal experience through art, play, movement, dance, drama, music, etc.
References:
Finlay, L. (2015). Relational integrative psychotherapy: Engaging process and theory in practice. John Wiley & Sons.
Psycologists for Social Responsibility (2002) Conference Report: Integrating Approaches to Psychosocial Humanitarian Assistance. Retreived from:http://www.psysr.org/about/pubs_resources/PsySR%20Maine%20Conference%20Report%202002.pdf
Gertel Kraybill, O. (2015) post – expressive psychosocial support. Expressive Trauma Integration. Retreived from: https://www.eti.training/single-post/2015/04/26/Guidelines-for-Expressive-Psychosocial-Support
Tags:





Comments